Bronchoscopy
What is Bronchoscopy?
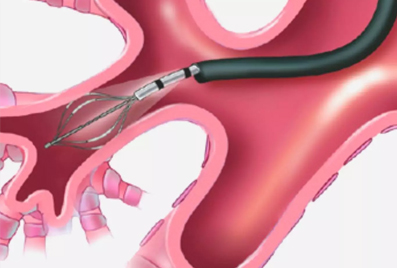
Bronchoscopy is a test to view the lungs’ airways and diagnose lung disease. A pulmonologist performs this test to look at your lungs and airways, collect samples of mucus or tissue, remove blockages from lungs or airways, or provide treatment for lung problems.
Bronchoscopy is performed by inserting a thin, flexible tube called a bronchoscope, through your nose or mouth, down the throat and windpipe, and into the airways. The physician will be able to see the larynx, trachea, bronchi, and bronchioles.
Flexible and rigid are the two types of bronchoscope, where the former is most commonly used as it can move into smaller airways. In case there is a lot of bleeding in the lungs, or large debris is stuck in the airways, the rigid bronchoscope may be used.
What is the need for Bronchoscopy?
Bronchoscopy is done to diagnose and treat lung disease. Your pulmonologist can inspect your airways, take a sample for biopsy, and even pass through special devices through the bronchoscope for some procedures.
Bronchoscopy is necessary to:
-
Diagnose lung disease
-
Remove mucus or foreign substances from your airways
-
Obtain a biopsy tissue from the lungs
-
Place a stent in the airways
-
Control bleeding in the bronchi
Bronchoscopy is also conducted if you have a persistent cough that has lasted for three months, or to check lymph nodes in the chest in case of lung cancer, or even diagnose inflammation, infection, and bleeding.
What are the risks of Bronchoscopy?
Generally, the flexible bronchoscope has fewer risks than the rigid bronchoscope. However, there are risks and complications involved with the procedure, the sedative, or the topical numbing medicine.
Some risks that the procedure may hold are:
-
Bleeding
-
Infection
-
Collapsed lung
-
Irritation in the airways or the vocal cords
-
Breathing difficulties
-
Fever
-
Sore throat
-
Low blood oxygen
The risks mainly depend on the patients’ general health and other conditions. Hence your physician will tell you the hazards that can occur and if you are eligible to take the test. You may not be able to take a bronchoscopy if you have:
-
Severe bleeding of narrowing of the trachea
-
Hazardous coughing
-
Low oxygen level
-
High blood pressure in the lungs’ blood vessels
How to prepare for Bronchoscopy?
Your physician will inform you of the details of the procedure beforehand. Do not forget to notify your provider of all the medications you take. You may need to stop specific medicines before the procedure.
Some preparation instructions include:
-
Avoid eating or drinking 6 to 8 hours before the procedure
-
Stop taking blood-thinning medications like aspirin and ibuprofen under the physician's order
-
You may be asked to remove your hearing aid, contact lens, and glasses
-
Arrange someone to take you back home and for certain work the next day